Why Experts Are Exploring New Ideas for Managing Chronic Fatigue
Chronic fatigue can affect energy levels, focus, and daily routines, and researchers are examining new ideas that may help people better understand their symptoms. Current discussions explore sleep patterns, stress responses, immune-system factors, and lifestyle influences that may contribute to ongoing exhaustion. Specialists are also reviewing pacing strategies, supportive routines, and emerging monitoring tools designed to track fluctuations throughout the day. This article summarizes the concepts gaining attention in fatigue research, offering an informative and neutral overview without medical promises.
Chronic fatigue syndrome represents one of the most perplexing health challenges facing modern medicine. Characterized by profound exhaustion that does not improve with rest and often worsens with physical or mental activity, this condition affects millions of Americans. Recent years have witnessed a shift in how medical professionals and researchers approach this complex syndrome, moving away from one-size-fits-all solutions toward more nuanced, individualized strategies that address the multifaceted nature of persistent tiredness.
What Does Fatigue Pattern Research Reveal About Energy Fluctuations
Recent investigations into fatigue patterns have uncovered significant variations in how individuals experience energy depletion throughout their day, week, and month. Researchers have identified that chronic fatigue often follows predictable cycles influenced by sleep quality, activity levels, and even seasonal changes. Studies utilizing wearable technology and detailed patient journals have mapped these energy fluctuations with increasing precision, revealing that many individuals experience post-exertional malaise—a worsening of symptoms following even minor physical or cognitive effort. This research has led to the development of personalized energy tracking systems that help patients identify their unique fatigue triggers and optimal activity windows. Understanding these patterns allows for better planning of daily tasks and social commitments, reducing the likelihood of energy crashes that can last days or weeks. The data collected through these studies continues to inform treatment protocols and provides validation for patients whose experiences have historically been dismissed or misunderstood.
How Do Lifestyle Influences on Energy Shape Daily Functioning
The relationship between daily habits and energy levels in chronic fatigue patients has become a focal point of contemporary research. Diet quality, hydration status, sleep hygiene, and environmental factors all contribute to the complex equation of energy availability. Nutritional studies have shown that certain dietary patterns may either support or undermine cellular energy production, though individual responses vary considerably. Sleep architecture analysis reveals that many chronic fatigue patients experience disrupted sleep cycles, even when total sleep duration appears adequate. Environmental considerations such as noise levels, light exposure, and temperature regulation also play underappreciated roles in energy management. Social interactions and emotional demands represent another dimension of lifestyle influences, with research indicating that psychological stress can directly impact physical energy reserves. Healthcare providers increasingly recommend comprehensive lifestyle assessments as part of initial evaluations, recognizing that sustainable energy improvements often require addressing multiple factors simultaneously rather than focusing on isolated interventions.
What Are the Connections Between Stress and Immune Insights
The intersection of psychological stress and immune system function has emerged as a critical area of investigation in understanding chronic fatigue. Research demonstrates that prolonged stress can dysregulate immune responses, potentially contributing to the inflammatory processes observed in many fatigue syndrome cases. Studies have documented elevated levels of certain inflammatory markers in chronic fatigue patients, alongside alterations in stress hormone patterns that differ from healthy controls. The hypothalamic-pituitary-adrenal axis, which governs stress responses, often shows abnormal functioning in individuals with persistent fatigue. Immune system studies have revealed changes in natural killer cell activity and cytokine production that may help explain the post-exertional symptom exacerbation many patients experience. These findings have prompted exploration of interventions targeting both stress reduction and immune modulation. Mind-body practices, cognitive behavioral approaches, and carefully monitored physical rehabilitation programs are being evaluated for their potential to restore more balanced stress and immune functioning. The growing recognition of these connections has validated patient reports of symptom worsening during stressful periods and has opened new avenues for therapeutic development.
How Do Pacing Strategies Help Conserve and Rebuild Energy
Pacing has emerged as one of the most widely recommended non-pharmacological approaches for managing chronic fatigue. This strategy involves carefully balancing activity and rest to avoid triggering post-exertional symptom flares while gradually building functional capacity. Unlike traditional graded exercise therapy, which has proven problematic for many chronic fatigue patients, pacing respects individual energy limitations and emphasizes sustainability over pushing through symptoms. Effective pacing requires developing awareness of early fatigue signals and responding proactively rather than waiting until exhaustion forces rest. Many practitioners now teach patients to break activities into smaller segments with built-in recovery periods, a technique sometimes called energy envelope management. The goal centers on maintaining relatively stable energy levels rather than experiencing the boom-and-bust cycles that characterize poorly managed chronic fatigue. Research into pacing effectiveness shows promising results, with many patients reporting reduced symptom severity and improved quality of life when consistently applying these principles. Digital tools and smartphone applications have made pacing more accessible by providing activity tracking, rest reminders, and personalized feedback based on individual patterns.
What Emerging Approaches Show Promise for Future Management
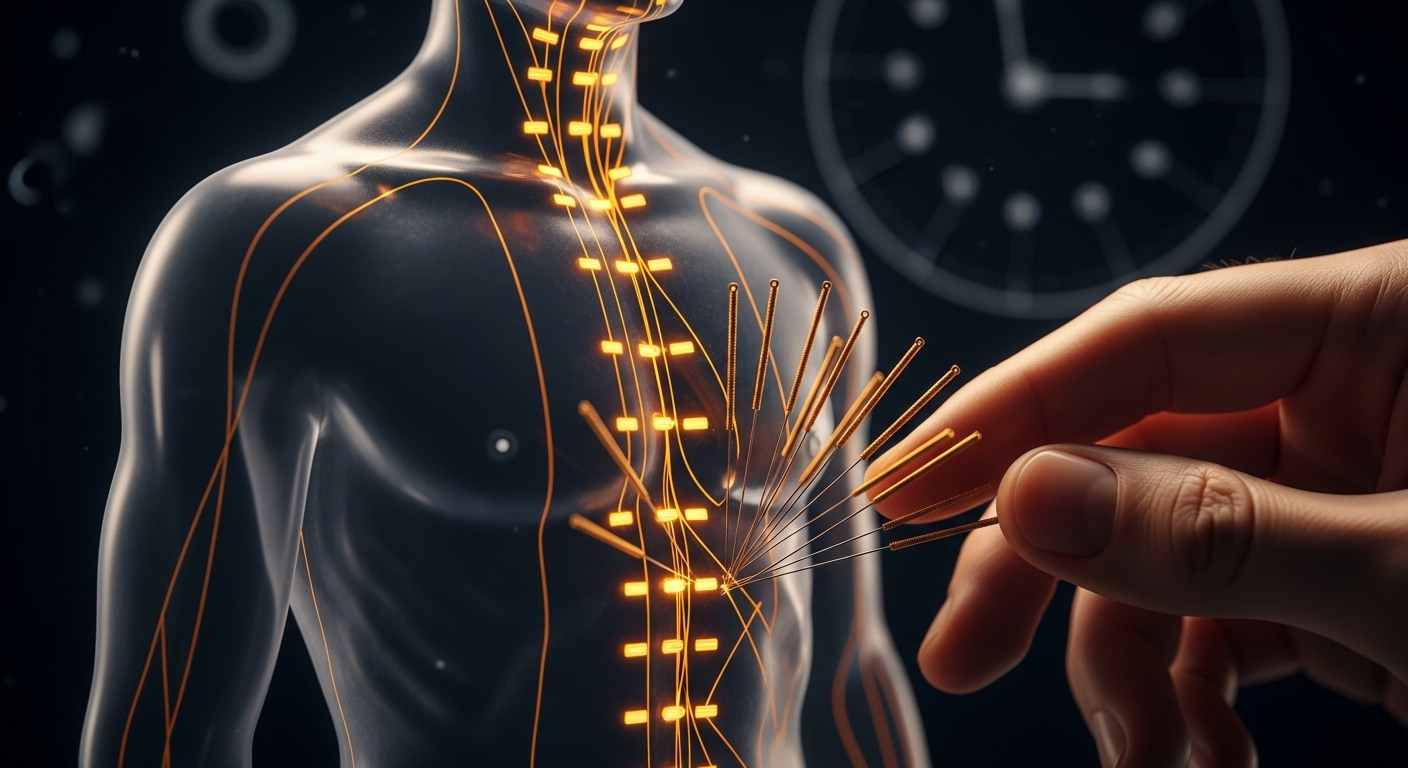
The landscape of chronic fatigue management continues to evolve as researchers explore novel interventions informed by advancing scientific understanding. Mitochondrial support strategies aim to address potential cellular energy production deficits through targeted nutritional supplementation and metabolic optimization. Autonomic nervous system retraining programs seek to restore balance to the body’s automatic regulatory functions, which often show dysregulation in chronic fatigue patients. Specialized physical therapy approaches adapted for this population focus on gentle movement that supports rather than depletes energy reserves. Complementary therapies including acupuncture, massage, and meditation practices are being systematically evaluated for their potential contributions to comprehensive care plans. Pharmacological research explores medications that might address specific underlying mechanisms such as neuroinflammation or mitochondrial dysfunction. Patient advocacy has driven increased research funding and clinical trial development, accelerating the pace of discovery. The shift toward viewing chronic fatigue as a legitimate medical condition requiring serious scientific attention represents significant progress, though substantial work remains to develop consistently effective treatments.
Conclusion
The exploration of new management approaches for chronic fatigue reflects growing recognition of this condition’s complexity and legitimacy. As research uncovers connections between fatigue patterns, lifestyle factors, stress responses, and immune function, patients gain access to more sophisticated tools for understanding and managing their symptoms. Pacing strategies and personalized interventions offer practical pathways toward improved quality of life, even as scientists continue searching for more definitive solutions. The ongoing commitment to investigating this challenging syndrome provides hope that future breakthroughs will transform management options and outcomes for those living with persistent exhaustion.




